Gingival Enlargement: Clinical Overview and Classification
Gingival Enlargement: Clinical Overview and Classification

Gingival Enlargement: Clinical Overview and Classification
Gingival Enlargement: Clinical Overview and Classification
Introduction
Gingival enlargement (also termed gingival overgrowth) refers to an abnormal increase in the size of the gingiva.
- These terms are clinical and descriptive, avoiding outdated and misleading terminology such as “hypertrophic gingivitis” or “gingival hyperplasia”.
- Gingival enlargement can result from a variety of causes, ranging from local inflammation to systemic disease or drug administration.
Classification of Gingival Enlargement
Gingival enlargements are generally classified according to etiologic factors and pathologic changes:
- Inflammatory Enlargement
- Chronic
- Acute
- Drug-Induced Enlargement
- Anticonvulsants
- Immunosuppressants
- Calcium channel blockers
- Enlargements Associated with Systemic Diseases/Conditions
- Conditioned Enlargement
➔ Pregnancy
➔ Puberty
➔ Vitamin C deficiency
➔ Plasma cell gingivitis
➔ Pyogenic granuloma (nonspecific conditioned enlargement) - Systemic Diseases
➔ Leukemia
➔ Granulomatous diseases (e.g., Wegener’s granulomatosis, sarcoidosis)
- Conditioned Enlargement
- Neoplastic Enlargement
- Benign tumors
- Malignant tumors
- False Enlargement
- Apparent increase in gingival mass due to underlying pathology (e.g., bone enlargement, exostosis).
Distribution of Gingival Enlargement
Enlargements are further described by location and distribution:
- Localized: Adjacent to a single tooth or group of teeth
- Generalized: Involving gingiva throughout the mouth
- Marginal: Confined to the marginal gingiva
- Papillary: Limited to interdental papillae
- Diffuse: Involving marginal, attached gingiva, and papillae
- Discrete: Isolated sessile or pedunculated, tumor-like enlargement
Grading of Gingival Enlargement
| Grade | Description |
|---|---|
| 0 | No signs of enlargement |
| I | Confined to interdental papilla |
| II | Involves papilla and marginal gingiva |
| III | Covers three-quarters or more of the crown |
Types of Gingival Enlargement
1. Inflammatory Enlargement
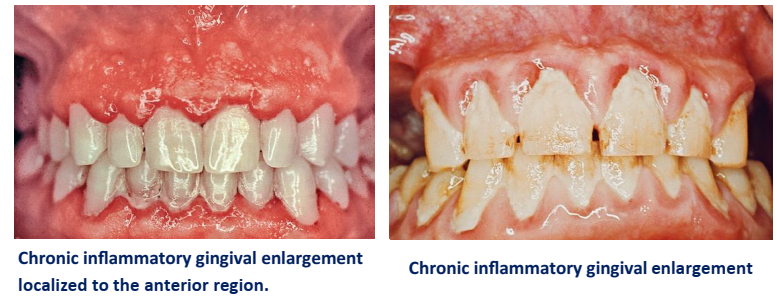
A. Chronic Inflammatory Enlargement
✔ Clinical Features
- Begins as a slight ballooning of interdental papilla and marginal gingiva.
- Creates a “life preserver–like” bulge that may extend to cover part of the crown.
- Usually slow-growing, painless, and may be localized or generalized.
- May appear as sessile or pedunculated tumor-like masses, which can enlarge, regress, and recur.
- Occasionally ulcerated at the fold between mass and adjacent gingiva.
✔ Etiology
- Caused by prolonged plaque exposure.
- Risk factors for plaque accumulation:
➔ Poor oral hygiene
➔ Anatomic irregularities
➔ Faulty restorations
➔ Orthodontic appliances
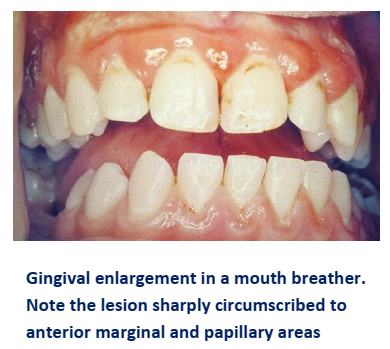
✔ Mouth Breathing and Gingival Changes
- Common in maxillary anterior region.
- Gingiva: red, edematous, shiny, and clearly demarcated from unaffected gingiva.
- Mechanism: likely due to surface dehydration irritation, though not conclusively proven.
✦ Clinical Example: A patient with open-mouth sleeping habit presents with edematous, shiny anterior gingiva, despite otherwise fair oral hygiene.
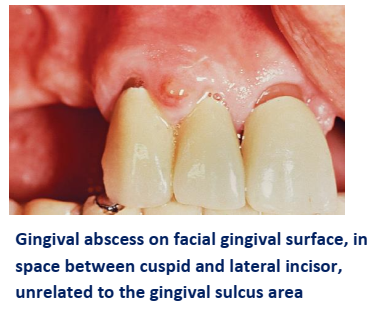
B. Acute Inflammatory Enlargement
Gingival Abscess
- Rapid onset, localized, painful, expanding lesion.
- Appears as red, shiny swelling, later becoming fluctuant with pus discharge.
- Often involves marginal gingiva or interdental papilla.
- Adjacent teeth may be percussion-sensitive.
Etiology
- Caused by foreign body impaction (e.g., toothbrush bristle, apple core, lobster shell).
- Must be distinguished from periodontal abscess, which involves deeper supporting tissues.
2. Drug-Induced Gingival Enlargement
Certain medications are strongly associated with gingival overgrowth.
✔ Common Groups of Drugs:
- Anticonvulsants (e.g., phenytoin, valproic acid)
- Immunosuppressants (e.g., cyclosporine, tacrolimus)
- Calcium channel blockers (e.g., nifedipine, amlodipine, diltiazem)
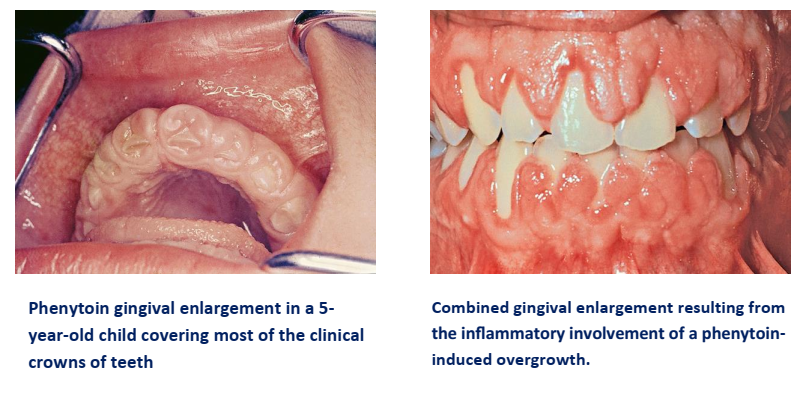
General Clinical Features
- Begins as bead-like, painless enlargement of interdental papilla.
- Progresses to involve marginal gingiva and may form massive folds covering crowns.
- Firm, pale pink, mulberry-shaped surface, usually non-bleeding when non-inflamed.
- Frequently complicated by secondary inflammation due to impaired plaque control.
- Typically generalized, but more severe in anterior regions.
- Absent in edentulous areas; regression occurs after extraction or discontinuation of drug.
Pathogenesis
- Interaction of fibroblasts, inflammation, and genetic predisposition.
- Hypothesis: fibroblasts in inflamed gingiva are more active and responsive to drugs.
- Plaque control reduces inflammation but does not prevent overgrowth.
A. Anticonvulsants
- Phenytoin (Dilantin) most common agent; enlargement in ~50% of users.
- Other drugs: ethotoin, mephenytoin, ethosuximide, valproic acid.
- Enlargement independent of dosage beyond a threshold.
- Proposed mechanisms:
➔ Fibroblast proliferation
➔ Increased glycosaminoglycan synthesis
➔ Reduced collagen breakdown
✦ Clinical Note: Phenytoin-induced enlargement more common in younger patients.

B. Immunosuppressants
- Cyclosporine:
➔ Enlargement in 25–70% of patients.
➔ More vascularized than phenytoin-related overgrowth.
➔ Magnitude linked to plasma concentration.
➔ Worse when combined with calcium channel blockers. - Tacrolimus: Similar immunosuppressive action but causes less gingival enlargement.

C. Calcium Channel Blockers
- Used for hypertension and cardiovascular disease.
- Drugs implicated: nifedipine, amlodipine, diltiazem, verapamil.
- Nifedipine: gingival enlargement in ~20% of users; severity may increase with cyclosporine.
- Enlargement may or may not be dose-dependent in humans.
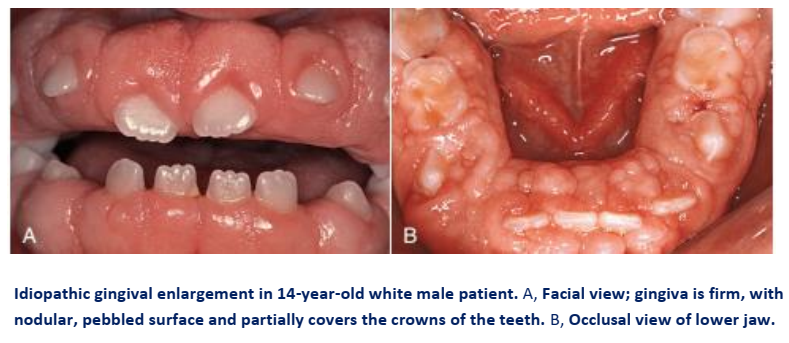
3. Idiopathic Gingival Enlargement
✦ Also called: gingivomatosis, elephantiasis, idiopathic fibromatosis, hereditary gingival hyperplasia, congenital familial fibromatosis.
Clinical Features
- Involves attached gingiva, gingival margin, and interdental papillae (unlike phenytoin overgrowth, often limited to margin + papilla).
- Affects both jaws (facial & lingual), but sometimes limited to one arch.
- Gingiva: pink, firm, leathery, minutely pebbled surface.
- Severe cases: teeth almost fully covered, enlargement protrudes into vestibule, jaws look distorted.
- Secondary inflammation at margins is common.
Histopathology
- Bulbous connective tissue increase, relatively avascular.
- Densely packed collagen bundles + many fibroblasts.
- Epithelium thickened, acanthotic with elongated rete pegs.
Etiology
- Cause unknown → “idiopathic.”
- Hereditary cases: autosomal recessive or autosomal dominant.
- May begin with eruption of primary or permanent dentition, sometimes regresses after extraction.
- Teeth/plaque may be initiating factors.
- Reported in tuberous sclerosis (epilepsy, mental deficiency, cutaneous angiofibromas).
4. Gingival Enlargements Associated with Systemic Diseases
Two mechanisms:
- Magnification of plaque-induced inflammation (Conditioned enlargements).
- Direct manifestation of systemic disease (independent of plaque status).
1. Conditioned Enlargements
These occur when systemic conditions exaggerate the gingival response to plaque.
A. Hormonal Enlargements
Pregnancy
- Due to ↑ progesterone & estrogen (10–30× normal by 3rd trimester).
- Mechanism:
➔ ↑ vascular permeability → edema, exaggerated inflammatory response
➔ Changes in microbiota (↑ Prevotella intermedia) - Marginal enlargement: generalized, bright red/magenta, friable, bleeds easily.
- Pregnancy tumor (pyogenic granuloma type):
➔ Appears after 3rd month (1.8–5% incidence).
➔ Mushroomlike, sessile/pedunculated, dusky red, smooth/glossy with pinpoint markings.
➔ Painless unless debris accumulates → ulceration. - Histopathology: Angiogranuloma → vascular connective tissue, engorged capillaries, fibrous stroma, thickened epithelium.
- Management: meticulous plaque control, calculus removal. Tissue removal alone → recurrence. Usually regresses after delivery.

Puberty
- Affects both sexes, mainly interproximal/marginal.
- Bulbous papillae, more pronounced on facial than lingual.
- Enlargement out of proportion to local plaque deposits.
- Peaks around ages 11–14; microbial role: Capnocytophaga, Prevotella intermedia, P. nigrescens.
- Histology: chronic inflammation, edema, degenerative changes.

B. Nutritional Enlargement (Vitamin C Deficiency – Scurvy)
- Not caused directly by deficiency, but modifies response to plaque.
- Gingiva: bluish-red, soft, friable, shiny surface, hemorrhagic, necrotic with pseudomembrane.
- Histology: chronic inflammation with acute superficial response, hemorrhage, collagen degeneration, scarce fibroblasts.

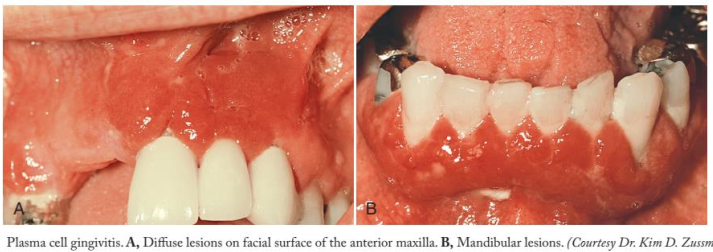
C. Allergic Enlargement (Plasma Cell Gingivitis)
- Marginal enlargement spreading to attached gingiva.
- Red, friable, granular, bleeds easily.
- Differentiated from plaque gingivitis by location and histology.
- Histology: epithelial spongiosis, damage in basal/spinous layers, dense plasma cell infiltrate.
- Possible allergen sources: chewing gum, dentifrices, foods.
- Resolves after allergen removal.
- Rare severe cases linked to rapidly progressive periodontitis.
- Solitary plasma cell tumor (plasmacytoma) occasionally in oral mucosa → usually benign but may indicate multiple myeloma.
D. Nonspecific Conditioned Enlargement (Pyogenic Granuloma)
- Exaggerated response to minor trauma.
- Clinically & microscopically similar to pregnancy tumor.
- Treatment: lesion removal + elimination of local irritants.
- Recurrence rate: ~15%.
2. Systemic Diseases Causing Gingival Enlargement
A. Leukemia
- Enlargement may be diffuse, marginal, localized, or generalized.
- Gingiva: bluish-red, shiny, moderately firm, friable, hemorrhagic.
- May ulcerate at gingival-tooth junction.
- Common in acute leukemia.
- Histology: dense immature leukocyte infiltration, chronic inflammation, engorged capillaries, necrotic pseudomembranous areas.
B. Granulomatous Diseases
- Wegener’s Granulomatosis
- Rare, involves respiratory tract, kidneys, vasculitis.
- Oral signs: mucosal ulceration, gingival enlargement, mobility, exfoliation, delayed healing.
- Gingiva: reddish-purple, bleeds easily.
- Histology: chronic inflammation, giant cells, microabscesses under thin acanthotic epithelium.
- Etiology: immune-mediated injury.+
- Prognosis improved with immunosuppressive drugs (>90% remission).
- Sarcoidosis
- Unknown etiology; young adults (20s–30s), more common in Black patients.
- Multiorgan involvement, including gingiva → red, smooth, painless enlargement.
5. NEOPLASTIC ENLARGEMENT (GINGIVAL TUMORS)
This section provides only a brief description of some of the more common neoplastic and pseudoneoplastic lesions of the gingiva. The reader is referred to texts on oral pathology for more comprehensive coverage.
Benign Tumors of the Gingiva
Epulis
- Epulis is a generic term used clinically to designate all discrete tumors and tumorlike masses of the gingiva.
- It serves to locate the tumor but not to describe it.
- Most lesions referred to as “epulis” are inflammatory rather than neoplastic.
Epidemiology
- Neoplasms account for a comparatively small proportion of gingival enlargements and make up a small percentage of the total number of oral neoplasms.
- In a survey of 257 oral tumors, approximately 8% occurred on the gingiva.
- In another study of 868 growths of the gingiva and palate, of which 57% were neoplastic and the remainder inflammatory, the following incidence of tumors was noted:
- Carcinoma: 11.0%
- Fibroma: 9.3%
- Giant cell tumor: 8.4%
- Papilloma: 7.3%
- Leukoplakia: 4.9%
- Mixed tumor (salivary gland type): 2.5%
- Angioma: 1.5%
- Osteofibroma: 1.3%
- Sarcoma: 0.5%
- Melanoma: 0.5%
- Myxoma: 0.45%
- Fibropapilloma: 0.4%
- Adenoma: 0.4%
- Lipoma: 0.3%
Fibroma
- Fibromas of the gingiva arise from the gingival connective tissue or from the periodontal ligament.
- They are slow-growing, spherical tumors that tend to be firm and nodular but may be soft and vascular.
- Fibromas are usually pedunculated.
- Hard fibromas of the gingiva are rare; most of the lesions diagnosed clinically as “fibromas” are inflammatory enlargements.
- The so-called giant cell fibroma contains multinucleated fibroblasts.
- In another variant, mineralized tissue (bone, cementum-like material, and dystrophic calcifications) may be found; this type of fibroma is called peripheral ossifying fibroma.
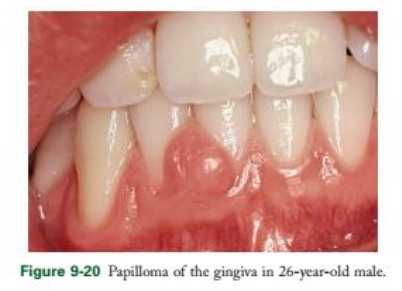
Papilloma
- Benign proliferations of surface epithelium, often (but not always) associated with human papillomavirus (HPV).
- Clinically: appear as solitary wartlike or cauliflower-like protuberances.
- They may be small and discrete or broad, hard elevations with minutely irregular surfaces.
Peripheral Giant Cell Granuloma
- Giant cell lesions of the gingiva arise interdentally or from the gingival margin.
- Most frequent on the labial surface.
- May be sessile or pedunculated.
- Appearance: ranges from smooth, regularly outlined masses to irregularly shaped, multilobulated protuberances with surface indentations.
- Occasionally ulcerated at the margin.
- Clinically: painless, variable in size, may cover several teeth.
- Consistency: firm or spongy.
- Color: pink to deep red or purplish blue.
Important Notes
- No pathognomonic clinical features; microscopic examination is required for definitive diagnosis.
- The prefix “peripheral” is needed to differentiate them from central giant cell granulomas (lesions originating within the jawbone).
- Some cases are locally invasive, causing destruction of underlying bone.
- Complete removal usually leads to uneventful recovery.
Central Giant Cell Granuloma
- Arises within the jaws and produces central cavitation.
- May create deformity of the jaw, giving the appearance of gingival enlargement.
Other Reported Tumors
- Mixed tumors (salivary gland type).
- Plasmacytomas of the gingiva (rare).

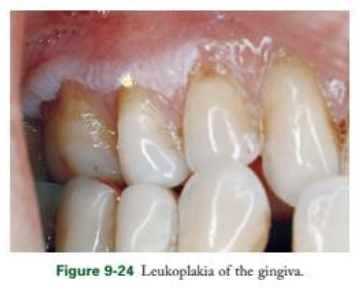
Leukoplakia
- Defined by WHO as a white patch or plaque that does not rub off and cannot be diagnosed as any other disease.
- Etiology: remains obscure, but associated with:
- Tobacco (smoke or smokeless)
- Candida albicans
- HPV-16 and HPV-18
- Trauma
- Clinical appearance: grayish-white flattened scaly lesion → thick, irregular keratinous plaque.
Malignant Potential
- 80% benign.
- 20% malignant or premalignant.
- 3% invasive carcinomas.
- Biopsy is mandatory, selecting the most suspicious area.
Gingival Cyst
- Usually microscopic, seldom clinically significant.
- When large enough: localized enlargements involving marginal and attached gingiva.
- Common in mandibular canine and premolar areas, most often lingual.
- Painless, but may cause erosion of alveolar bone with expansion.
- Must be differentiated from lateral periodontal cyst (intraosseous, developmental in origin).
- Histogenesis: from odontogenic epithelium or implanted surface/sulcular epithelium.
- Treatment: removal → uneventful recovery.
Sarcoma
- Rare in gingiva.
- Types reported: fibrosarcoma, lymphosarcoma, reticulum cell sarcoma.
- Kaposi’s sarcoma: often seen in AIDS patients, especially in palate and gingiva.
Metastasis to Gingiva
- Rare occurrence.
- Reported primary sites:
- Colon adenocarcinoma
- Lung carcinoma
- Melanoma
- Renal cell carcinoma
- Hypernephroma
- Chondrosarcoma
- Testicular tumors
Clinical Reminder
- Low incidence of oral malignancy must not mislead clinicians.
- Any gingival tumor, tumorlike lesion, or ulceration unresponsive to therapy should be biopsied and examined microscopically.
6. FALSE ENLARGEMENT
False enlargements are not true gingival enlargements but result from increases in the size of underlying osseous or dental tissues. Clinically, the gingiva may appear normal aside from the bulk increase.
A. Underlying Osseous Lesions
- Causes:
- Tori and exostoses
- Paget’s disease
- Fibrous dysplasia
- Cherubism
- Central giant cell granuloma
- Ameloblastoma
- Osteoma
- Osteosarcoma
- Gingiva may appear normal or may have unrelated inflammatory changes.
B. Underlying Dental Tissues
- During eruption stages (esp. primary dentition), labial gingiva may show bulbous marginal distortion.
- Caused by bulk of gingiva overlying enamel prominence.
- Termed developmental enlargement.
- Often persists until junctional epithelium migrates to cementoenamel junction.
Clinical Note
- Developmental gingival enlargements are physiologic and usually harmless.
- If complicated by marginal inflammation → appears as extensive gingival enlargement.
- Treatment: manage inflammation, not surgical resection.




