Anatomy of the Periodontium
🦷 Anatomy of the Periodontium
👉 Anatomy of the Periodontium MCQs
The oral mucosa consists of three main zones:
📌 Masticatory mucosa – gingiva and hard palate.
📌 Specialized mucosa – covering the dorsum of the tongue.
📌 Lining mucosa – covering the rest of the oral cavity.
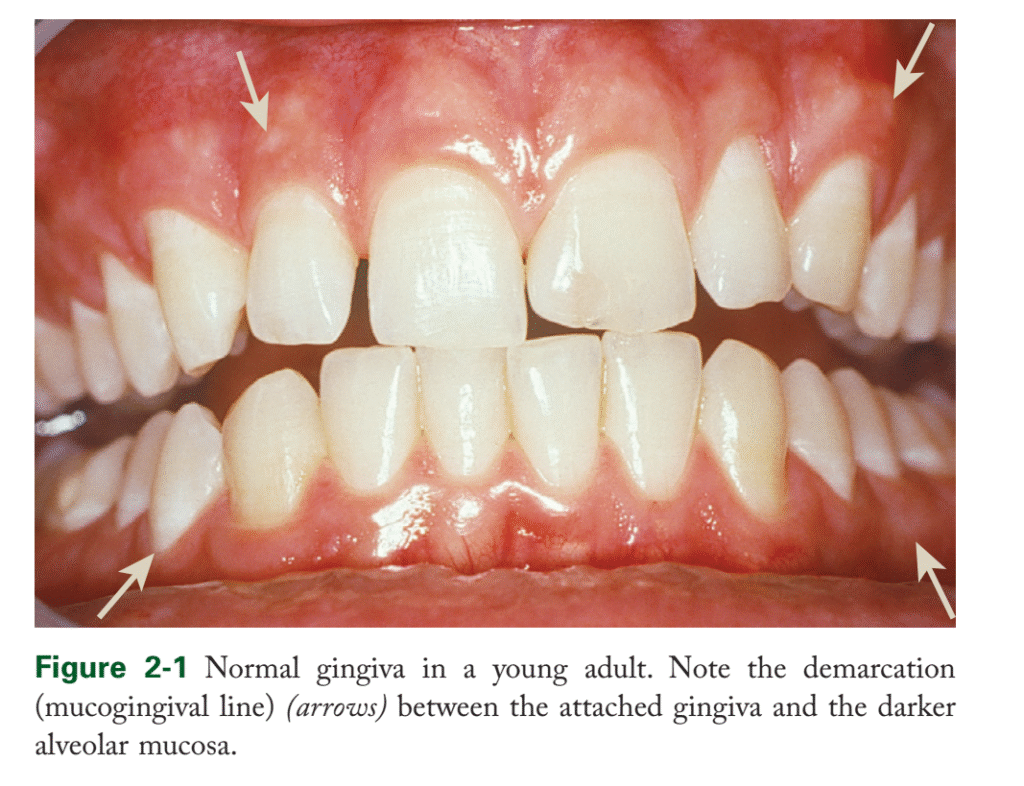
The gingiva is the part of the oral mucosa covering the alveolar processes and surrounding the necks of teeth.
🩺 Clinical Features of Gingiva
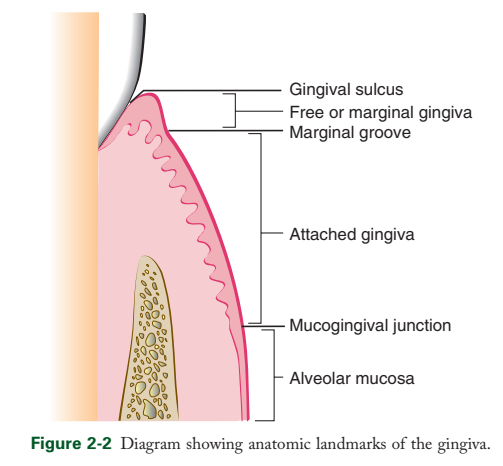
In adults, normal gingiva covers the alveolar bone and tooth root slightly above the cementoenamel junction (CEJ). Gingiva is anatomically divided into:
🔹 Marginal (free) gingiva
• Forms the soft tissue wall of the gingival sulcus.
• Unattached and surrounds teeth like a collar.
• Sometimes demarcated from attached gingiva by the free gingival groove (~1 mm wide).
🔹 Gingival Sulcus
• Shallow V-shaped space between the tooth surface and free gingival epithelium.
• Depth is a key diagnostic parameter:
• Ideal depth: ~0 mm (experimental/germ-free conditions).
• Normal human gingiva: 0.69–1.8 mm histologically.
• Clinically measured probing depth: 2–3 mm.
🔹 Attached Gingiva
• Continuous with marginal gingiva, firm and resilient.
• Tightly bound to the alveolar bone’s periosteum.
• Demarcated by the mucogingival junction.
• Width varies:
• Maxilla: 3.5–4.5 mm (incisors), 1.9 mm (first premolars).
• Mandible: 3.3–3.9 mm (incisors), 1.8 mm (first premolars).
• Changes occur due to age, supraeruption, or recession.
🔹 Interdental Gingiva
• Fills the interproximal space beneath tooth contacts.
• Shapes:
• Pyramidal – tip under contact point.
• Col-shaped – valley connecting facial and lingual papillae.
💡 Key Points
• Gingiva is a protective barrier against mechanical and microbial damage.
• Different types of gingiva have distinct histology and thickness for their function.
• Probing depth is clinically more relevant than histologic depth.
• Attached gingiva is crucial for periodontal stability; width varies by location and age.
• Interdental papilla shapes are clinically significant for esthetics and plaque control.
👉 Anatomy of the Periodontium MCQs
🦠 Microscopic Features of Gingiva
Gingiva is composed of:
• Stratified squamous epithelium – overlying protective layer.
• Connective tissue core – mainly collagen fibers and ground substance; less cellular.
These two components work together to provide mechanical support and defense against infection.
🧬 Gingival Epithelium
• General Function
• Provides a physical barrier and participates actively in host defense.
• Responds to bacteria by proliferation, signaling, differentiation, and controlling tissue homeostasis.
• Anatomic Areas
📌 Oral (outer) epithelium – faces the oral cavity.
📌 Sulcular epithelium – lines the gingival sulcus.
📌 Junctional epithelium – attaches epithelium to the tooth surface.
• Principal Cells
• Keratinocytes – main cell type, proliferate in basal layer and differentiate as they migrate superficially.
• Non-keratinocytes – Langerhans cells, Merkel cells, melanocytes; contribute to immune defense and sensory function.
⚙️ Keratinization & Differentiation
• Basal cells divide by mitosis; some cells migrate superficially.
• Keratinization involves:
1. Cell flattening with increased tonofilaments.
2. Formation of intercellular junctions and keratohyalin granules.
3. Disappearance of nuclei in fully keratinized cells.
• Types of epithelium:
• Orthokeratinized – fully keratinized, no nuclei in surface layer.
• Parakeratinized – nuclei retained in surface cells; granules dispersed.
• Non-keratinized – no granular or corneal layers; surface cells have nuclei.
• Keratin Proteins
• Basal cells produce lower-molecular-weight keratins (e.g., K19).
• Higher-molecular-weight keratins (e.g., K1) appear as cells migrate.
🔬 Cell Connections & Ultrastructure
• Desmosomes – connect keratinocytes, tonofilaments anchor here.
• Tight junctions (zonae occludens) – allow passage of ions and small molecules.
• Organelles – mitochondria abundant in deeper layers, decrease superficially.
• Keratin granules (Odland bodies) – involved in keratinization and intercellular cementation.
🧪 Non-Keratinocyte Cells
• Melanocytes – in basal/spinous layers, produce melanin in melanosomes.
• Langerhans cells – dendritic, antigen-presenting, located in suprabasal layers; contain Birbeck granules.
• Merkel cells – in deeper layers, connected to nerve endings; function as tactile sensors.
🧱 Basal Lamina & Connective Tissue Interface
• Basal lamina: lies beneath basal epithelial layer.
• Composed of:
• Lamina lucida – mainly laminin; hemidesmosomes attach here.
• Lamina densa – type IV collagen.
• Anchoring fibrils – connect lamina to underlying connective tissue; loop around collagen fibers (~750 nm).
• Functions as barrier to particulate matter but allows fluid exchange.
💡 Key Points
• Gingival epithelium actively participates in immune defense.
• Keratinocyte proliferation and differentiation maintain barrier integrity.
• Non-keratinocyte cells play critical roles in immunity and sensation.
• Basal lamina and anchoring fibrils connect epithelium to connective tissue and maintain structural stability.




